The Challenge!
Offer in the International market, customized Advanced NDT solutions, in specific technical areas, where competitors fails.
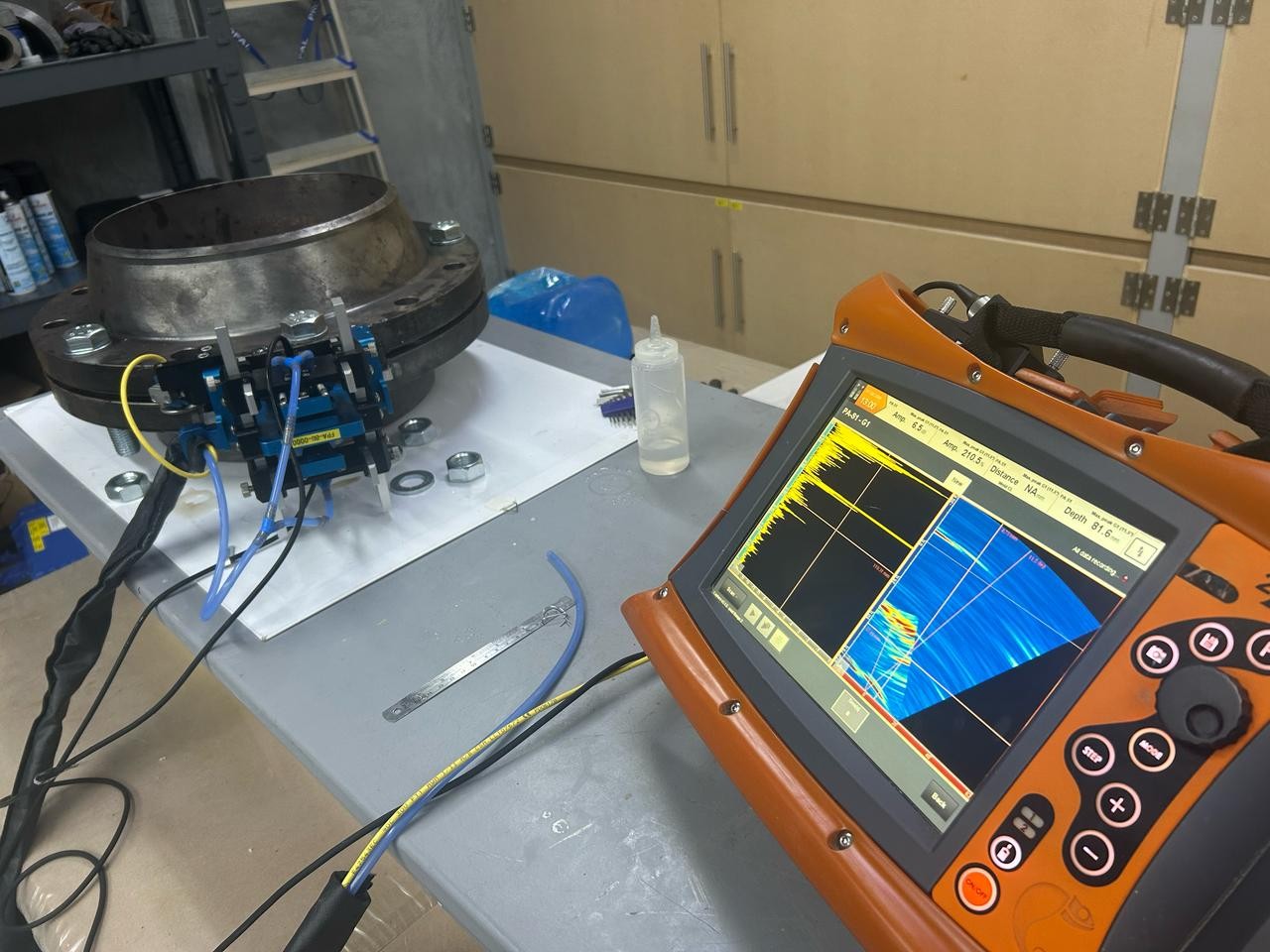
We aspire to solve high profile technical problems, as we are not just using the existing market technology, but we are developing in our Labs, our own technology and solutions, mainly in the field of Advanced UT.